Guide to Nutrition for Autism: Manage GI & ASD Symptoms
- Introduction: Decoding the Gut-Immune-Brain Triad
- When Meltdowns are Physiological Signals
- The “Golden Duo” and the IL-1β Marker
- Defeating Fermentation with Digestive Enzymes
- The Fiber Paradox and Vitamin A Deficiency
- Opioid Excess and the Redox Balance
- PHGG and Microbiome Modulation
- Nutrition Guide for Autism: The 101Autism Strategic Roadmap
- Conclusion: A Shift in the Clinical Paradigm
- Clinical Considerations & FAQ for Caregivers
- References
TL;DR: Clinical Strategy at a Glance
- The GI Range: Gastrointestinal (GI) symptoms affect between 9% and 91% of autistic children. These are not merely comorbid issues but are biologically linked to the severity of core symptoms.
- The Synergistic Duo: Evidence for Omega-3 alone is weak, but the combination of Vitamin D and Omega-3 significantly improves social communicative functioning, particularly in “immune responders” with elevated baseline IL-1β.
- Mechanistic Interventions: Targeted strategies—including saccharide-digesting enzymes (papain/pepsin), low-FODMAP protocols, and microbial modulators like PHGG—aim to restore homeostasis by downregulating proinflammatory signaling.
- The Precision Roadmap: Management must transition from “behavioral compliance” to a multidisciplinary medical model using validated tools like the Rome criteria and the ASD-specific GI symptom inventory.
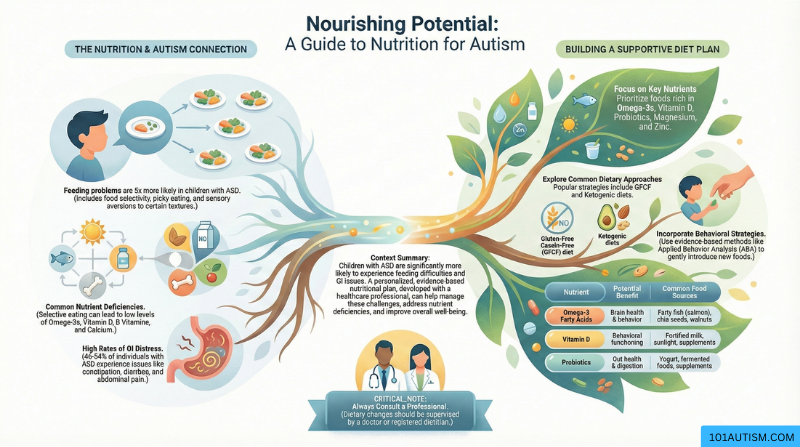
This comprehensive guide to nutrition for autism provides evidence-based strategies to help parents and caregivers manage gastrointestinal symptoms and improve behavioral outcomes in children with autism spectrum disorder (ASD). Understanding the critical connection between gut health and autism symptoms is essential for developing an effective nutritional approach tailored to your child’s unique needs.
Introduction: Decoding the Gut-Immune-Brain Triad
For the caregiver, a sudden sensory meltdown or period of unexplained irritability is often the most exhausting hurdle of the day. As a clinical strategist, I view these not as “behavioral noncompliance,” but as physiological signals. We are now operating within the framework of the gut-immune-brain triad—a bidirectional communication system where gut dysbiosis drives intestinal inflammation, subsequent neuro-immune dysregulation, and sensory sensitivities. When we identify a “vicious circle” of abdominal pain and enzyme deficiencies, we move beyond management and toward biological healing.
When Meltdowns are Physiological Signals
Clinical data indicates that children with Autism Spectrum Disorder (ASD) are four times more likely to experience GI symptoms than neurotypical peers, with a prevalence range of 9–91%. Constipation is the most prevalent manifestation, often increasing in likelihood as verbal and social impairments become more severe.
Because of limited verbal ability and abnormal sensory perception, many children cannot localize pain. Instead, GI distress manifests as:
- Aggression and self-injury: Physical outlets for internal visceral discomfort.
- “Abdominal pressure” behaviors: Leaning over furniture or objects to mitigate pain.
- Sleep and psychiatric disruptions: 80% of autistic children face sleep abnormalities, often exacerbated by GERD or lower GI tract discomfort.
Clinical Insight: We must stop misinterpreting dietary refusal or withdrawal as “pickiness.” These are potential indicators of underlying medical conditions, such as digestive enzyme deficiencies or intestinal hyperpermeability.
The “Golden Duo” and the IL-1β Marker
While 57% of children with ASD are Vitamin D deficient, supplementation is most effective when combined with Omega-3 polyunsaturated fatty acids (PUFAs). This combination targets the TLR4/NF-κB proinflammatory signaling pathways.
- Mechanistic Precision: The most significant improvements in social communicative functioning occur in children with elevated IL-1β at baseline. These “immune responders” benefit from the PUFA-driven suppression of Th17 differentiation and the promotion of anti-inflammatory IL-10.
- Social Outcomes: The synergy of Vitamin D and Omega-3 yields significant improvements in social awareness and communicative functioning that neither supplement achieves alone.
Defeating Fermentation with Digestive Enzymes
GI dysfunction in ASD is frequently linked to intestinal deficiencies in glycoside hydrolase and polysaccharide lyase. When these enzymes are insufficient, undigested sugars ferment in the gut, leading to osmotic diarrhea, bloating, and flatulence.
Supplementation with saccharide-digesting enzymes—specifically papain and pepsin—has demonstrated more than just digestive relief. By reducing the byproduct of fermentation, clinical trials show an amelioration of core ASD symptoms, including improved emotional regulation and a decrease in repetitive behaviors.
The Fiber Paradox and Vitamin A Deficiency
While fiber is the standard recommendation for constipation, the “Fiber Paradox” suggests that for sensory-hypersensitive children, high intake of complex carbohydrates can backfire, causing bloating and flatulence that increases irritability.
- The Low-FODMAP Strategy: Limiting fermentable carbohydrates can downregulate TLR4-mediated signaling and restore mucosal barrier function. However, this must be balanced carefully to avoid depleting beneficial Bifidobacteria.
- The Vitamin A Factor: We must address the “selective eating” trap. Vitamin A deficiency is a major exacerbator of core symptoms and increases the risk of celiac disease and IBD by impairing retinal dehydrogenase activity and gut barrier integrity.
Opioid Excess and the Redox Balance
The “Opioid Excess Theory” posits that dietary peptides (gluten and casein) can act as opioids in the brain due to a hyper-permeable “leaky” gut. This activates the morphine-serotonin system, disrupting redox homeostasis and even altering DNA methylation processes.
- The Camel Milk Alternative: Camel milk is a promising clinical intervention because it contains lower casein than cow’s milk and is rich in protective antioxidants like glutathione and superoxide dismutase, which directly address oxidative stress in the gut-brain axis.
PHGG and Microbiome Modulation
Restoring the microbiome is about more than “adding good bacteria.” Modulators like Partially Hydrolyzed Guar Gum (PHGG) work by reducing serum proinflammatory cytokines and selectively promoting beneficial taxa like Bifidobacteria while suppressing detrimental species like Candida. Candida overgrowth is particularly concerning as it contributes to hyperserotonemia, impeding brain serotonin synthesis from tryptophan and exacerbating neurobehavioral symptoms.
Nutrition Guide for Autism: The 101Autism Strategic Roadmap
To effectively manage the nutritional and GI landscape of ASD, I recommend this two-step clinical algorithm:
Step 1: Identify and Address Obstacles
- Screening with Precision: Utilize the Rome criteria for general GI signs and the ASD-specific GI symptom inventory to capture non-verbal indicators like abdominal pressure or rigid-compulsive behaviors.
- Multidisciplinary Integration: A team must include a pediatric gastroenterologist, a clinical dietitian, and a psychiatrist to differentiate between biological deficits and behavioral issues.
Step 2: Targeted Nutritional Management
- Tailored Diets: Match the intervention to the pathology (e.g., SCD for carbohydrate malabsorption, Low-FODMAP for mucosal barrier restoration).
- Strategic Delivery: To maximize efficacy and tolerability, consider subcutaneous B12 injections instead of oral versions to circumvent GI adverse effects.
- Longitudinal Monitoring: Track nutrient trajectories, specifically monitoring serum 25(OH)D3 and retinol levels, to prevent the developmental delays associated with restrictive eating.
Conclusion: A Shift in the Clinical Paradigm
Nutritional management in ASD is shifting away from “fad diets” and toward precision nutrition. By viewing every “behavioral” challenge as a potential signal from the gut-immune-brain triad, we move toward restoring gut homeostasis as a foundational pathway for functional independence.
Final Strategic Thought: If we viewed every ‘behavioral’ challenge as a potential signal from the gut, how would our approach to care change today?
——————————————————————————–
Clinical Considerations & FAQ for Caregivers
Is the GF/CF diet a universal requirement? No. Its efficacy is context-dependent. While it addresses the “opioid excess” model, it is most beneficial for children with documented sensitivities or GI comorbidities. Indiscriminate use can lead to fiber deficiency and worsened constipation.
What are the primary risks of restrictive nutritional strategies? The primary risks include nutritional imbalances—specifically Vitamin A and D deficiencies—and the depletion of beneficial gut flora. Highly restrictive diets can also exacerbate pre-existing eating disorders and disordered eating behaviors.
Can supplements cause secondary GI distress? Yes. Oral B12, iron, carnitine, and even certain digestive enzymes have been associated with GI side effects in susceptible individuals. This is why a strategic, monitored approach is essential.
What is the most common indicator of GI distress in non-verbal children? Constipation is the most prevalent symptom. In non-verbal children, this often manifests as increased social withdrawal, physical aggression, or self-injury rather than a direct complaint of pain.
——————————————————————————–
References
- Wu, Y., et al. (2025). “Gastrointestinal health and nutritional strategies in autism spectrum disorder.” PMC.
- Madra, M., et al. (2020). “Gastrointestinal issues and Autism Spectrum Disorder.” Child Adolesc Psychiatr Clin N Am.
- Jiang, Y., et al. (2023). “Omega-3 polyunsaturated fatty acids and/or vitamin D in autism spectrum disorders.” Frontiers in Psychiatry.
- Vissoker, R. E., et al. (2015). “Eating and feeding problems and gastrointestinal dysfunction in ASD.” Research in Autism Spectrum Disorders.
Discover more from Living with Autism
Subscribe to get the latest posts sent to your email.

